Lab 4: Pre-Lab
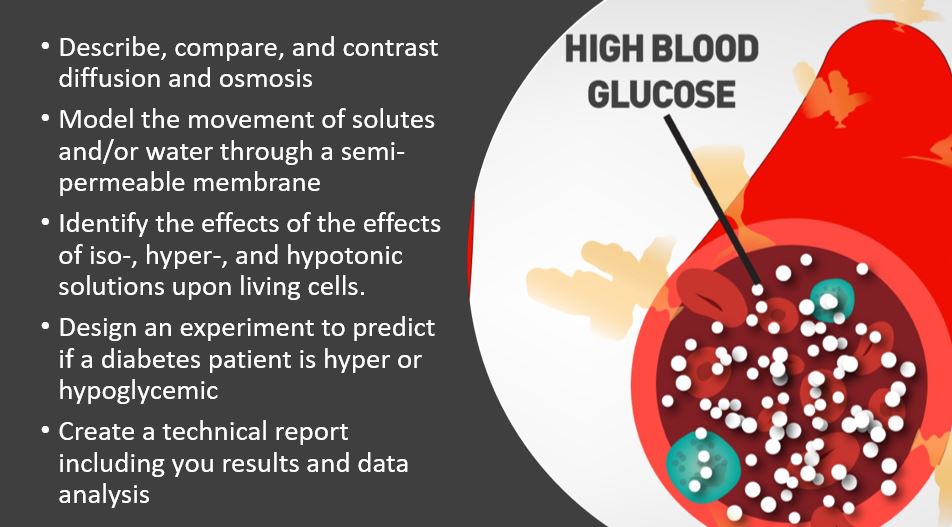
We have already learned a lot about the disease itself and the role glucose plays in diabetes. This lab will focus on the biochemistry behind some the symptoms of diabetes and necessitates further understanding of macromolecules (carbs, lipids and proteins) and of cells. You will explore diffusion and the insulin transduction pathway. You will conduct a series of tests to evaluate the effects of disruption of this pathway in diabetics.
-
Introduction
-
Do you know enough?
-
What will we do in lab?
-
LABridge
<
>
1) How does glucose get into our cells?

Review the types of transport above. Make sure you understand which is which. Brainstorm some potential characteristics that may make it less likely for a substances to move via diffusion alone.
2) Do you know what happens in individuals with Type 2 Diabetes?
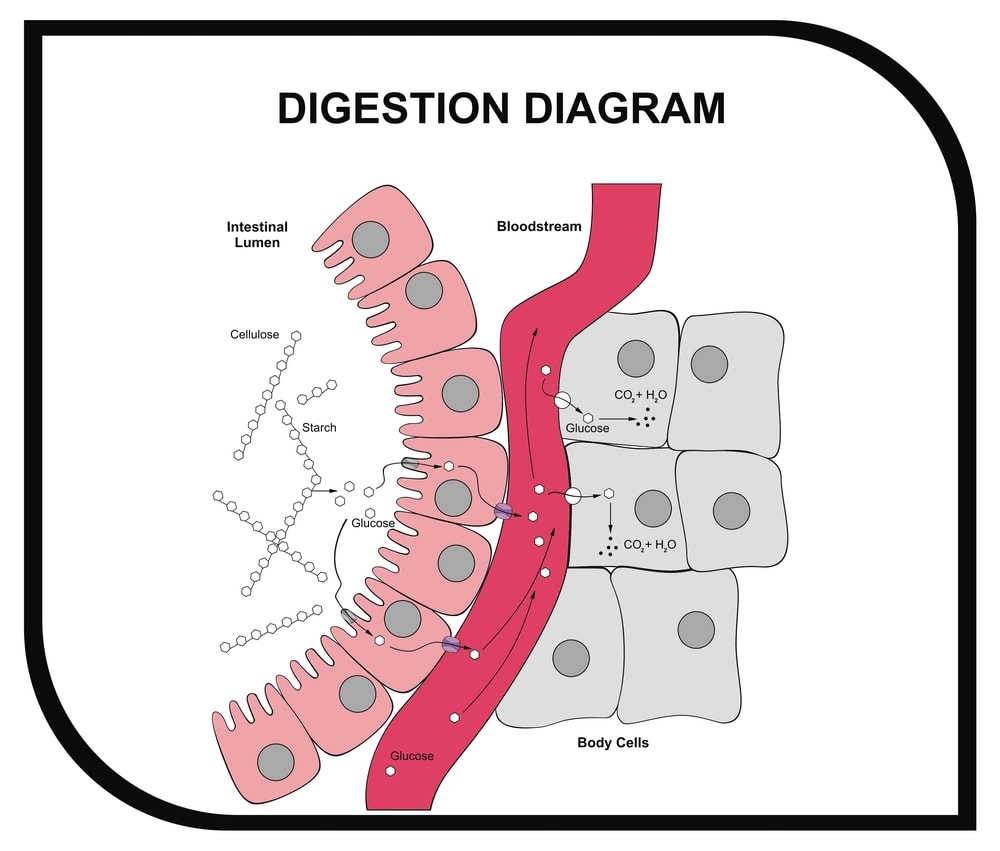
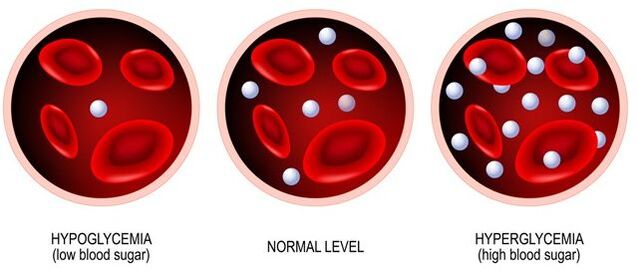
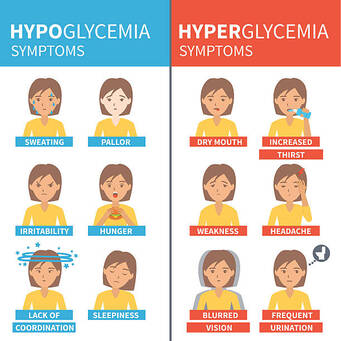
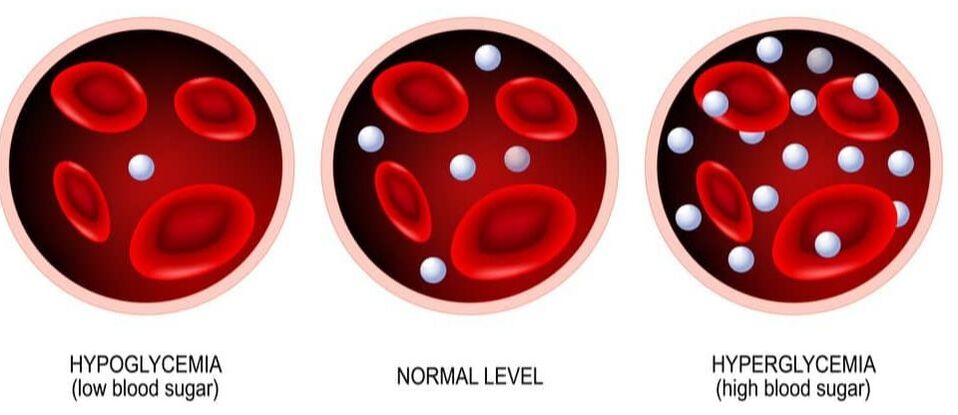
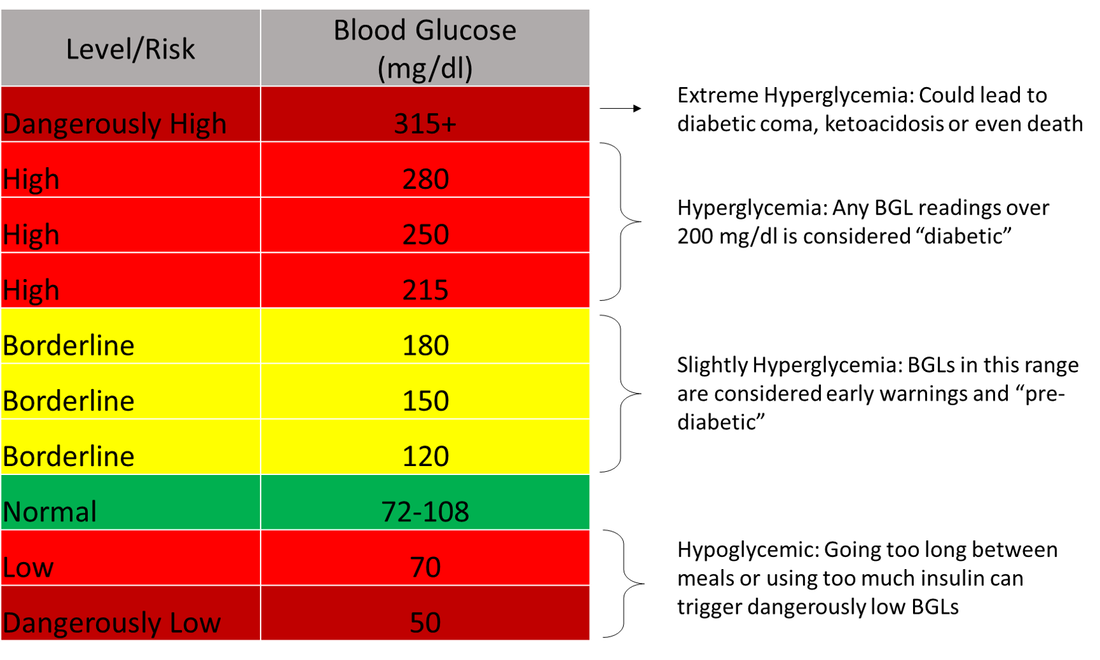
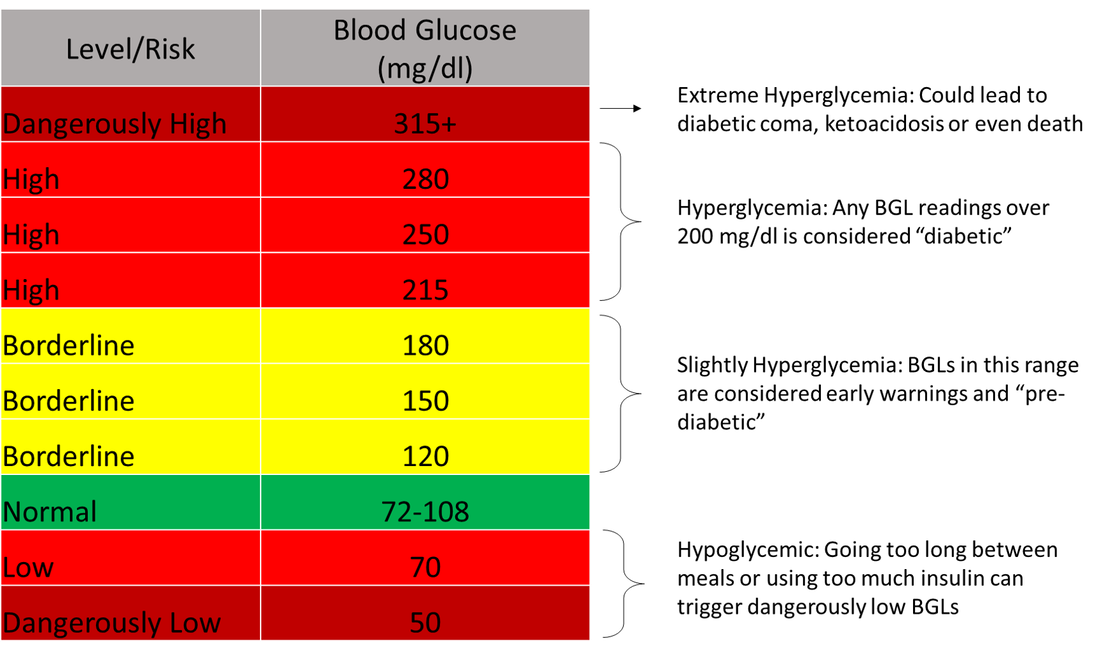
What happens if glucose doesn't get into the cell? The effect is an increased concentration of glucose in the blood. This establishes a concentration gradient, with higher concentrations of glucose outside the cell than inside the cell, a condition referred to as hyperglycemia. As diabetics often use artificial insulin (which we will discuss later) to regulate their blood sugar, they can also experience extremely low blood sugar due to insulin dosing and diet. This condition is known as hypoglycemia. In both conditions, osmosis will occur in an attempt to regulate the in-balance and maintain homeostasis.
3) What will we do in lab and how will we do it?
|
Lab 4 will proceed in three parts.
1) Predict the glucose concentration of two samples from 2 different patients: In the lab you will be provided with
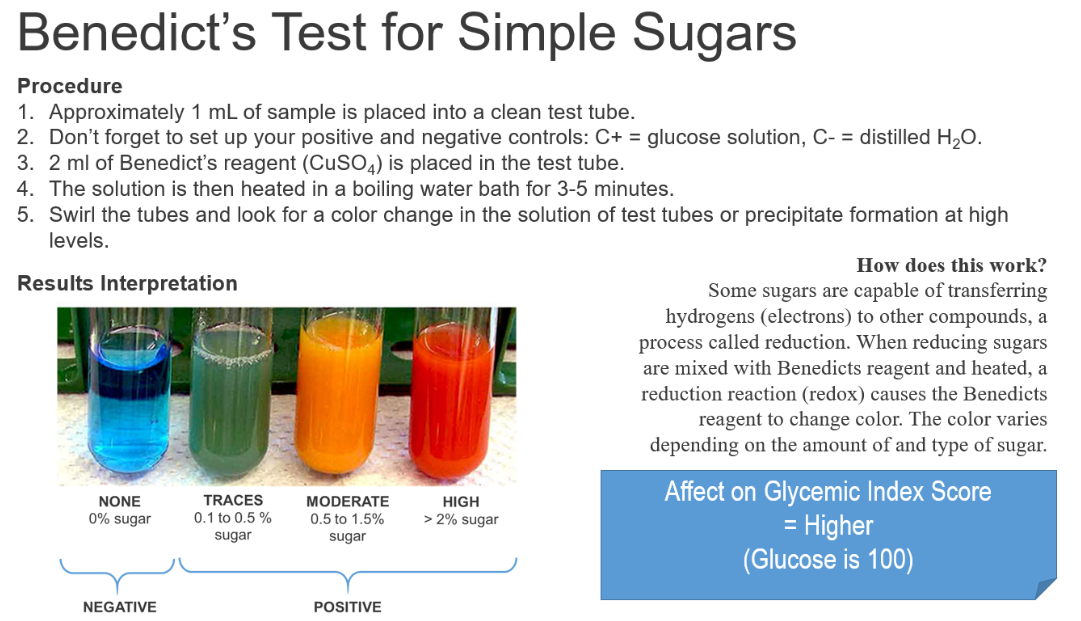
2) Determine the glucose level of the samples: You will accomplish this by using changes in mass, the Benedict's tests for simple sugars (from Lab 3), and Glucose Testing Strips. You will compare the results to your predictions. 3) Review signal transduction pathways: If it's hard or impossible for glucose to move across the membrane of some cells, how does it get in? We will research this pathway and the vital role it plays in diabetes. |
Lab 4: ProtocolIn today's lab you analyse variables that can affect the diffusion potential of a molecule. You will explore signal transduction pathways to understand the role they play in diabetes. Lastly, you will design an experiment which relies on the principles of osmoregulation to predict the condition of diabetic patients.
Exercise I. Predict the glucose concentration of two samples. Exercise II. Compare predictions with testing strips Exercise III. Review signal transduction pathways |
-
Exercise I
-
Exercise II
-
Exercise III
<
>
Exercise I. Predict the condition of diabetic patients: Hyper or Hypoglycemic?
As you read in the Pre-Lab, insulin enters our cells in several ways. The most important pathway is the insulin transduction pathway (which you will learn more about in Exercise III). This pathway is disrupted in diabetics either because insulin doesn't bind to the receptor or the receptor isn't activated upon binding. Regardless of the cause, the effect is an increased concentration of glucose (solute) in the blood. When this happens water moves into and out of cells attempting to reach an equilibrium, a process called osmoregulation.
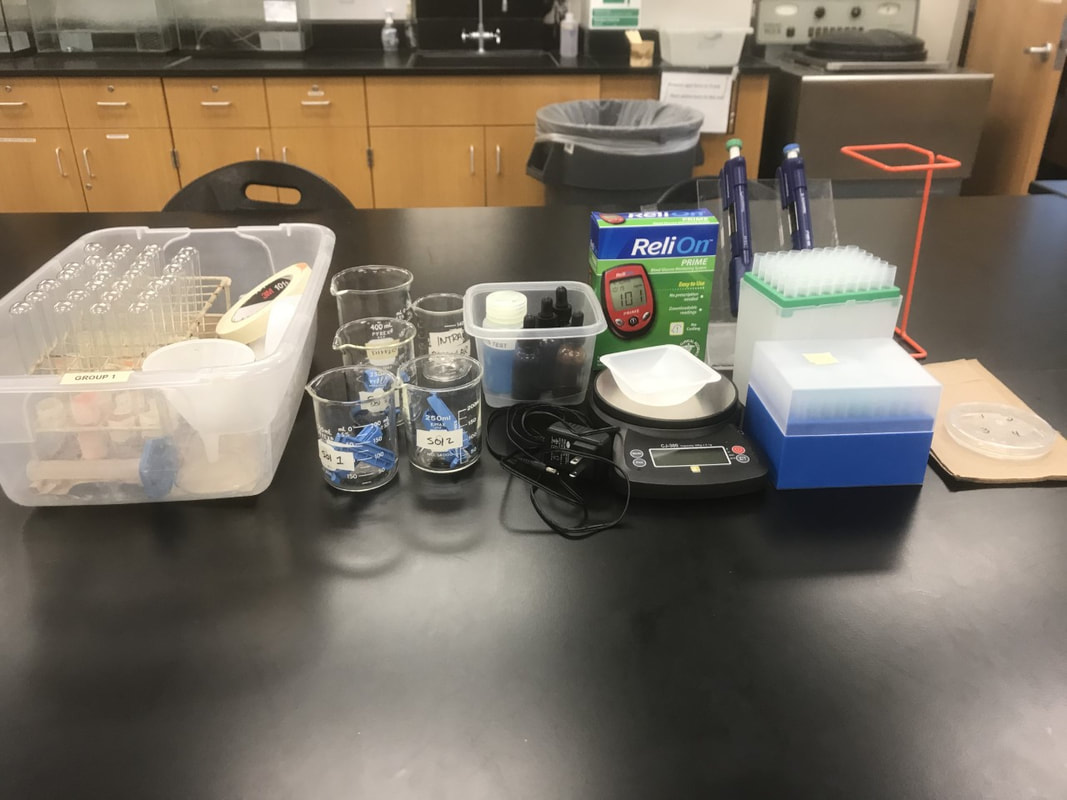
Materials: Your Tool Kit
|
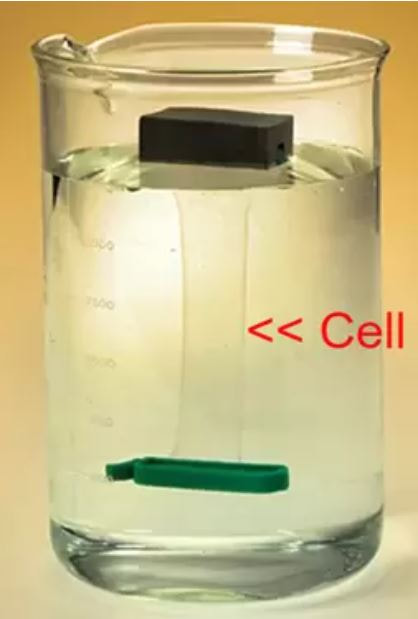
In this experiment you are going to use the water loss or water gain of an artificial "cell" to predict the status of the extracellular environment (e.g., hypertonic or hypotonic) and the condition of each patient (hyperglycemic or hypoglycemic).
|
Procedure
|
Exercise II. Test your predictions
|
Procedure: Test 1
Procedure: Test 2
|
|
|
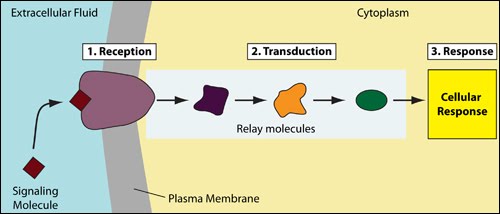
Exercise III. Explore the insulin transduction pathway
What does the evidence from our Pre-Lab, Exercise I and your research tell you about glucose? For some cells, an alternate pathway to simple diffusion is required. Specifically, some cells need to employ a signal trandsuction pathway to actively transport glucose when there are high concentrations in the blood.
|
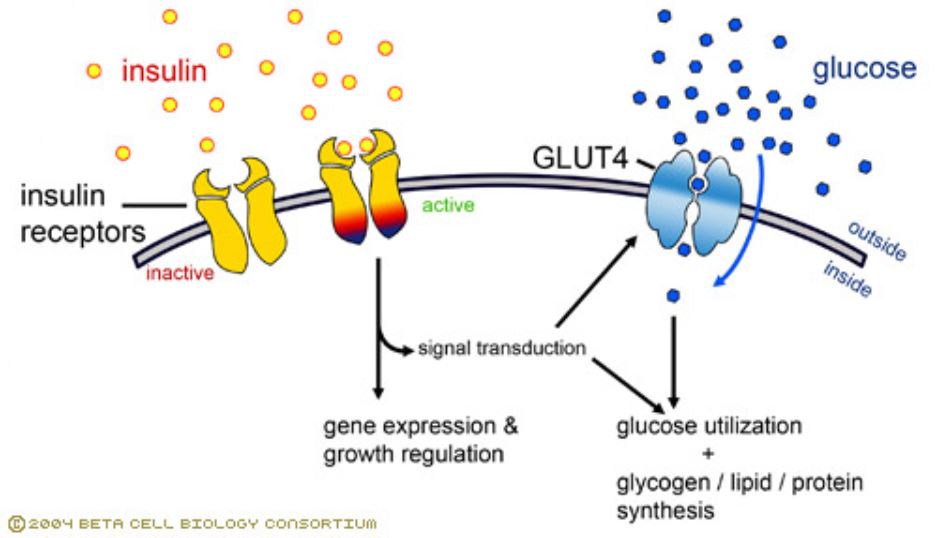
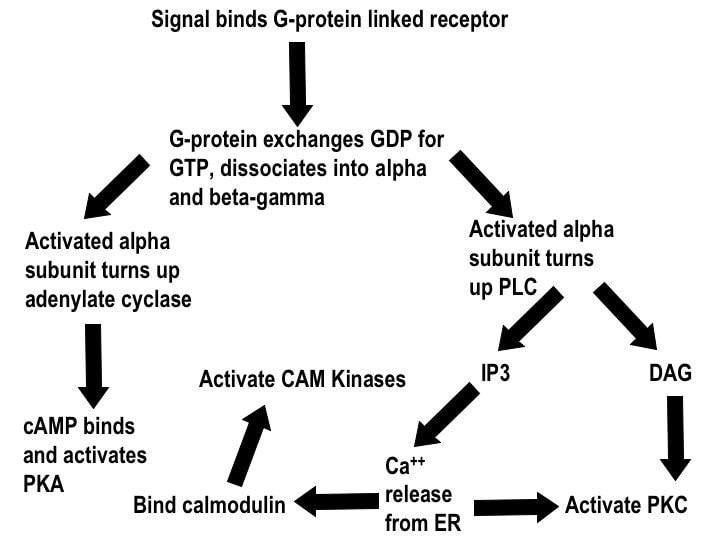
Signal transduction is imperative for cell-to-cell signaling. These biochemical pathways convert an extracellular signal to an intracellular signal, thus passing messages across our bodies. Transduction pathways occur when a signaling molecule binds to the surface of a cell, and its signal is then transferred and converted through a series of events to reach a target inside the cell, and cause the intended response.
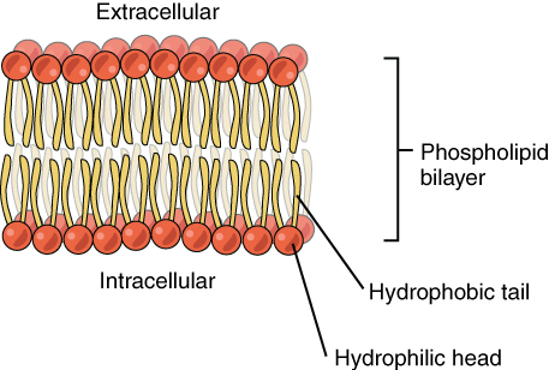
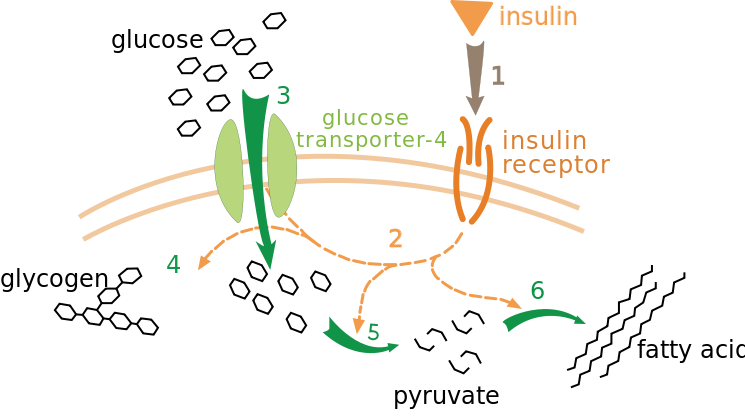
Insulin is a signaling molecule secreted by the pancreas when blood glucose levels are high. Insulin is a peptide hormone, in-soluble in lipids, and therefore cannot cross the cell membrane. Instead, a transduction pathway is required. In the pathway, insulin binds to a receptor in the cell membrane which triggers glucose uptake into the cell by a glucose transporter (typically GLUT-4). This uptake eventually decreases blood glucose levels. A transduction pathway is required for this to occur because:
Insulin is not required for all types of glucose uptake, but is required for muscle and fat tissues. Insulin-mediated glucose uptake is the pathway most responsible for blood sugar regulation. Procedure
If you finish early, work on your report. LAB 2 Exercise III. has all the details. |
|
Lab 4 BIOL 120 CONNECTIONS Section 6.2: Phospholipid Bilayers Section 6.3: How Substances Move Across Lipid Bilayers: Diffiusion & Osmosis Section 6.4: Proteins Alter Membrane Structure & Function Section 11.3: How do Distant Cells Communicate? Section 41.4: Nutritional Homeostasis Glucose as a Case Study |
Faculty Spotlight: Dr. Ajay Srivastava

Email: [email protected]
|
The Srivastava lab uses fruit flies (Drosophila) to better understand cell development and disease. Dr. Srivastava is particularly interested in the connection between the Extracellular Matrix (ECM) and the production and formation of tumors. The ECM is a dense network that connects the phospholipid bi-layer to the external cellular environment and is vital in cell structural support, growth and signaling. Just as our understanding of the cell membrane helps in the treatment of diabetes, Dr. Srivastava hopes that expanding our knowledge of the ECM can augment our understanding of cancer (Lab Web Page). He is always looking for talented and interested undergrads to help with his research! Check here for available positions. |
KAS citation format:
Mountjoy, N.J 2021. Title of page. Biological Concepts: Cells, Metabolism & Genetics. https://www.121cellmetagen.com. Date accessed (MM/DD/YYY).
Mountjoy, N.J 2021. Title of page. Biological Concepts: Cells, Metabolism & Genetics. https://www.121cellmetagen.com. Date accessed (MM/DD/YYY).